| Medicina | Medicina veterinara | Muzica | Psihologie | Retete | Sport |
Medicina
|
|
Qdidactic » sanatate & sport » medicina The role of thoracic electrical bioimpedance in the control of high blood pressure |
The role of thoracic electrical bioimpedance in the control of high blood pressure
The role of thoracic electrical bioimpedance in the control of high blood pressure
Abstract
Background: Even if important therapeutic progress has been made, the control of blood pressure (BP) values is far from being satisfactory, the target BP being reached in only 25% of the hypertensive patients treated.
Purpose of the study: To assess whether the use of the HOTMAN monitoring and hemodynamic management system could contribute to a better control of hypertension.
Methods: 56 hypertensive patients treated, but with no control of BP under their previous medication, were investigated by electrical bioimpedance using the HOTMAN system. The follow-up period was of 3 months. Four sets of hemodynamic assessments have been made during this time interval - at baseline and at one-month follow-up. We tried to obtain the normotensive, normodynamical status for every patient, whether by modulating the previous therapy or by adding new antihypertensive drugs according to the hemodynamic profile.
Results: At enrollment, 14,25% patients were under monotherapy, 64,28% were administered 2 antihypertensive drugs and 21,42% followed a triple therapy. After the first set of hemodynamic measurements, most of the patients had hypervolemia (82,14%) and/or vasoconstriction (67,85%) and/or hyperinotropy (37,%). The treatment was modulated for every patient according to his/her hemodynamic disorder. The treatment modulation was made according to each patient's hemodynamic disorder. Most patients (78,57%) suffered changes of the therapeutic strategy at the first hemodynamic assessment and after the first month of treatment. All patients received more than one drug: 42,85% received 2 antihypertensive drugs; 41,07% received 3 antihypertensive drugs and 16,07% received 4 antihypertensive drugs. A few number of patients had drug side effects (12,5%). At the end of the follow-up period, the BP values were controlled in 83,92% of the enrolled patients.
Conclusions: in order to treat hypertension as a hemodynamic disorder and not only as a simple manometric increase of the BP values, we managed to obtain the control of BP values in more than 80% of our patients after 1-2 medical examinations. Every patient received the best therapeutic strategy and appropriate doses, saving time and optimizing the costs. By adjusting therapy to each patient's personal hemodynamic profile, we had a limited percent of side effects.
Key words: BP control, normodynamic, hemodynamic management system.
INTRODUCTION
Hypertension could be considered the most frequent disease because of the big number of hypertensive people all around the world, exceeding one billion. The concepts regarding the hypertension definition have changed a lot lately, as well as its role as risk factor of arteriosclerosis and the BP target level to be reached. The relation between blood pressure (BP) and the risk of cardiovascular events is continuous and independent of other risk factors1. The increase of BP values is correlated with the increase of the risk of myocardial infarction, heart failure, cerebrovascular accident or kidney impairment. For people aged between 40 and 70, each increase by 20 mmHg of the systolic blood pressure or by 10 mmHg of the diastolic blood pressure doubles the risk of cardiovascular disease whichever the baseline value of the blood pressure, from 115/75 to 185/115 mmHg1.
Hypertension is currently considered the most important risk factor for cardiovascular diseases. Not treated, ~ 50% of the hypertensive patients die from coronary accidents or heart failure, ~ 33% from cerebrovascular accident and ~ 10-15% from kidney impairment≤. Despite all the therapeutic progresses made in the last decades, the blood pressure control is far from being satisfactory, reaching in Romania ~ 13% (according to the preliminary results of the epidemiological survey SEPHAR, under progress), but in the most developed countries as well, onlya percentage of maximum 27% of the treated patients, percentage that has remained almost unchanged in the last years (table 1)≥.
Country |
Percent of BP |
|
Australia |
19 % |
|
Canada |
16 % |
|
Great Britain |
5,9 % |
|
Finland |
20,5 % |
|
India |
9 % |
|
Scotland |
17,5 % |
|
Spain |
20 % |
|
USA |
27,4 % |
|
Zaire |
2,5 % |
Control defined as BP < 140/90 mmHg
Table 1: Hypertension global control
In the current medical practice, the hypertension treatment is frequently oriented only according to blood pressure values. Except for hypertensive patients with associated disorders who have specific treatment indications according to current guides, the choice of antihypertensive agent class is made most of the time according to the clinician's preferences or experience. The very guide ESH/ESC 2003 makes no reference to the baseline agent, considering that any BP reduction determines the increase of the global risk, whichever the selected drug4.
|
From physio-pathologic point of view, there is a series of various, often intricate mechanisms, involved in the occurrence of high BP values, which determine the increase of the heart output or of the peripheral vascular resistance. The increased intravascular volume5, the hyperinotropy6 and the vasoconstriction7 are the most important among them. Such mechanisms may react independently or together in each patient generating a specific hemodynamic profile. All these hemodynamic parameters (intravascular volume, vasoactivity, inotropy, chronotropy) are in a mutual relation and determine the heart output. Any therapeutic agent that reacts on other factors than those pathologically modified shall change the patient's hemodynamic balance, generating dysfunctional compensatory reactions. The consequences are the resistance to treatment (by compensatory mechanisms that oppose the drug action) and side effect such as fatigue, headaches, digestive disorders, impotency (by change of the hemodynamic balance). So the treatment purpose in a hypertensive patient needs to include normotension (normal manometric values of the blood pressure), as well as the obtaining of a normal blood flow, that is of the normohemodynamic status.
Literature data show that the hypertension therapy guided by hemodynamic parameters obtained through non-invasive methods - thoracic electrical bioimpedance - increases the rate of the hypertension control to 63%5.
PURPOSE
The study purpose is to assess whether the use of the hemodynamic monitoring and management system HOTMAN F100, HEMO SAPIENS INC could contribute to a better control of hypertension through the selection of the optimum antihypertensive therapy, specific to each client depending on the hemodynamic profile.
MATERIAL AND METHOD
The hemodynamic monitoring and management system HOTMAN uses the method of the thoracic electrical bioimpedance (BET). The term bioimpedance refers to the tissue resistance when crossed by high frequency and low magnitude electrical current. The method principle relies on the fact that the blood is the best electrical conductor of the human body. The electrical current used for measurements circulates between two pairs of electrodes located one in the upper part of the laterocervical region and the other at the level of the upper abdomen, parallel to the spinal column.† As the alveoli are filled with air (non-conducting medium), the electrical current is conducted mainly through the thoracic aorta and the venae cavae. Other four receptor-electrodes are located at the base of the laterocervical region and at the diaphragm level. They register the electrocardiogram as well as the voltage of the electrical current that crosses the thorax, which is proportional to the thoracic impedance. As this current is directed by the blood flow through the venae cavae and the thoracic aorta, it means that the blood flow variations are translated in variations of the thoracic impedance.
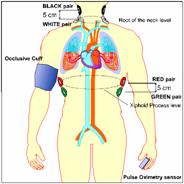
By entering demographic data and BP values at the examination moment, a series of hemodynamic parameters can be then automatically calculated, according to which the patient's hemodynamic status is determined: vasoactivity, volemia, inotropy, chronotropy, whose variation from the normal values is given as a percentage. As the electrodes also detect the EKG signal, other parameters can be measured as well: the pre-injection period (PIP), the ejection period (EP), the ventricular ejection time (VET), the systolic volume, the ejection fraction (figure 1A). Thus, the thoracic electrical bioimpedance may have an important role in the determination of the heart output through a non-invasive, continuous method, which offers cardiodynamic data in just in few minutes after the patient was connected. The hemodynamic status is graphically indicated under the form of a hemodynamic map, obtained through the simultaneous measurement of the systolic index (represented horizontally) and of the average blood pressure (ABP - represented vertically)(figure 1B). The patient's hemodynamic point will be situated at the intersection of the values and ABP, whose ideal values are 47 ml/m2 and 85 Torr. The hemodynamic map is obtained by crossing the upper and lower limits of the normal values of the two indices (35<SI<65 ml/m2 and 70<MAP<105 Torr); it will thus have nine hemodynamic classes. But among all, only one corresponds to the therapeutic purpose - the normohemodynamic status.
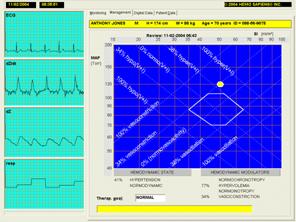
A B
Fig. 1 : A - cardiodynamic data obtained by non-invasive monitoring through BET ;
B - hemodynamic map (management page)8
So the normohemodynamic status requires the simultaneous presence of normotension and of normodynamic circulation. Based on the non-invasive measurement of the heart output and on the hemodynamic management map for each patient, we can identify hemodynamic anomalies - deviation percentage of volemia, inotropy, vasoactivity and chronotropy as compared to normal level. Thus, the antihypertensive therapy shall aim to normalize these parameters and to perform not only the blood pressure control, but also the hemodynamic normalization through an optimum treatment specific to each patient.
56 hypertensive patients were enrolled in our study, with uncomplicated high blood pressure, with no associated clinical conditions, in order to avoid a medication imposed by guides. All patients were already following an antihypertensive treatment, but were not controlled under the previous medication (BP values >140/90 mmHg clinically and >125/80 mmHg average of 24 hours on automatic outpatient monitoring). Each patient was investigated through the method of the thoracic electrical bioimpedance using the HOTMAN system. The follow-up period was of 3 months and meanwhile four sets of hemodynamic measurements were performed - upon enrollment in the study and then at one-month intervals. The intravascular volume, the inotropy, the vasoactivity, the chronotropy, the BP level and the global blood flow were determined. The target for each patient was to obtain the normodynamic normotensive status. This was obtained by modulation of the previous therapy or by addition of new anti-hypertensive agents depending on each patient's hemodynamic profile.
RESULTS:
The gender distribution showed a slight female dominance - 57,14%. The average age of the group patients was 56 7 years. At enrolment in the study, 14,25% of patients were under monotherapy, most of them - 64,28% - were administered two antihypertensive and 21,24% were under a triple therapy (fig.2).
Fig. 2 : Number of antihypertensive agents at enrolment in the study
After the first set of hemodynamic measurements, most of patients had hypervolemia (82,4%) and/or vasoconstriction (67,85%) and/or hyperinotropy (37,5%).
The treatment modulation was made according to each patient's hemodynamic disorder. At patients where the main hemodynamic change was hypervolemia we added a diuretic in the treatment (hydrochlorotiaside or indapamide) or we increased the diuretic doses, if a diuretic was already included in the treatment strategy or we reinforced the recommendation of a hyposodic diet. Patients with vasoconstriction received as part of the therapeutic strategy an ACE inhibitor as vasodilator agent, whose dose was maximally increased; later, if vasoconstriction remained as hemodynamic change, we added a calcium channel blocker such as dihydro-pyridine. In patients with hyperinotropy we associated a beta-blocker or we increased doses to patients whose therapy already included the beta-blocker. Drugs that did not correspond the patients' hemodynamic profile were excluded from treatment. Most of the patients (78,57%) suffered changes of the therapeutic strategy at the first hemodynamic determination and after the first treatment month (figure 3).
Figure 3 : Therapy changes after the first or second hemodynamic measurement
At the end of the study period, all patients were receiving polytherapy: 42.85% - 2 agents, 41.07% - 3 agents and 16.07% - 4 antihypertensive agents (figure 4).
Figure 4: Comparison between the number of antihypertensive agents at
enrolment and
at 3-month interval
The number of patients who experienced side effects was low (12,5%) and such effects were due mainly to the biochemical characteristics of the drugs used and not to hemodynamic disequilibrium.
At the end of the 3 follow-up months, the blood pressure values were controlled at a percentage of 83.92% of the subjects enrolled in the study (figure 5).
Figure 5: High blood pressure control after 3 months
DISCUSSIONS
Despite all the therapeutic availabilities of the last years in the field of high blood pressure, at the enrollment in our study, the blood pressure of patients who were taking two or even three efficient antihypertensives was not well controlled. In the absence of hemodynamic information, the clinician cannot assess the cause of lack of response to treatment, in the case of compliant patients. A significant percentage of patients presented from hemodynamic point of view increased peripheral vascular resistance, hard to assess in the current practice. In addition, the presence of hypervolemia in most of the patients (some of them treated with diuretic), in the absence of edema or other clinical signs of volemic overload, indicated the need of a more intense therapy, with more focus on the volemia control. The hemodynamic management system helped identify the causes of the lack of therapeutic control (vasoconstriction, hypervolemia, hyperinotropy).
The selection of therapeutic agents based on the hemodynamic profile specific to each patient and the non-invasive repeated measurements led to a better control of hypertension in this prospective study. The use of the hemodynamic monitoring and management system HOTMAN in the treatment of hypertension contributed to the BP control in most of the patients enrolled in the study, the result being clearly superior to those in literature. But we have to mention that in studies whose purpose was to reach the target blood pressure values, the BP control was obtained in a quite high percentage - up to 2/3 of the patients in the ALLHAT study[i]. Even compared to these results, the hemodynamic management of the high blood pressure may make a difference.
In the current study, hypertensive patients under treatment were examined, whose BP values were not well controlled. This shows an increased level of resistance at the conventional treatment then in patients enrolled in big clinical trials. The fact that all patients were under polytherapy at the end of our study leads to the same conclusion. We don't have to ignore the reduced sizes of the lot as well as the reduced duration of the patients' follow-up in the current study.
The side effects occurred in a reduced number of patients and few of them were of hemodynamic nature. On the long run this may lead to an increase of the compliance to treatment - aspect that was not researched in the current study. Big end points such as mortality and cardiovascular events, which could be improved through a superior hemodynamic balance, could not be studied either.
CONCLUSIONS
The results of this study indicate a gain from the point of view of the BP control in patients who follow a hemodynamic therapy. Hypertension should be treated as hemodynamic disorder and not only as a mere manometric increase of the BP values. By this approach with the same kind of drugs as in the conventional treatment, but used depending on each patient's hemodynamic profile, superior results are obtained from the point of view of the blood pressure as well as of the adverse events. The method has the advantage of a quick, non-invasive determination, with no risks. The method of hypertension hemodynamic management can determine the optimum therapeutic strategy and the appropriate dosing for each patient, by saving time and optimizing costs. To pertinently answer the question "How big is this gain?" it is necessary to conduct studies on bigger lots and with a longer follow-up period.
BIBLIOGRAPHY:
1. The Seventh Report of the Joint National Committee on
Prevention, Detection, Evaluation and Treatment of High Blood Pressure; The
2. Braunwald's† Cardiovascular Disease, seventh edition, chapter 37.
3. Mancia G, Grassi G - Eur Heart J 1999; suppl L:14-19
4. 2003 European Society of Hypertension - European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertension, 2003;21:1011-1053.
5. Shramek B.Bo., Tichy J.A., et al: Normohemodynamic goal-oriented antihypertensive therapy improves the outcome. The American Society of Hypertension, 11th Scientific Meeting, New York, 1996.
6. Weiberger MH,Fineberg NS,Fineberg SE, Weinberger M: Salt sensitivity, pulse pressure and death in normal and hypertensive humans. Hypertension 37:429, 2001.
7. Kim JR, Kiefe CI, Liu K, et al: Heart rate and subsequent
blood pressure in young adults: The
8. Shramek B.Bo - Sistemic Hemodynamics and Hemodynamic Management, 2002
9. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group: Major outcomes in high-risk hypertensive patients randomized to ACE inhibitors or calcium channel blocker versus diuretic. JAMA 288:2981, 2002.
| Contact |- ia legatura cu noi -| | |
| Adauga document |- pune-ti documente online -| | |
| Termeni & conditii de utilizare |- politica de cookies si de confidentialitate -| | |
| Copyright © |- 2025 - Toate drepturile rezervate -| |
|
|
|||
|
|||
|
|||
Referate pe aceeasi tema | |||
|
| |||
|
|||
|
|
|||